1. Hello, Shame
Episode Synopsis
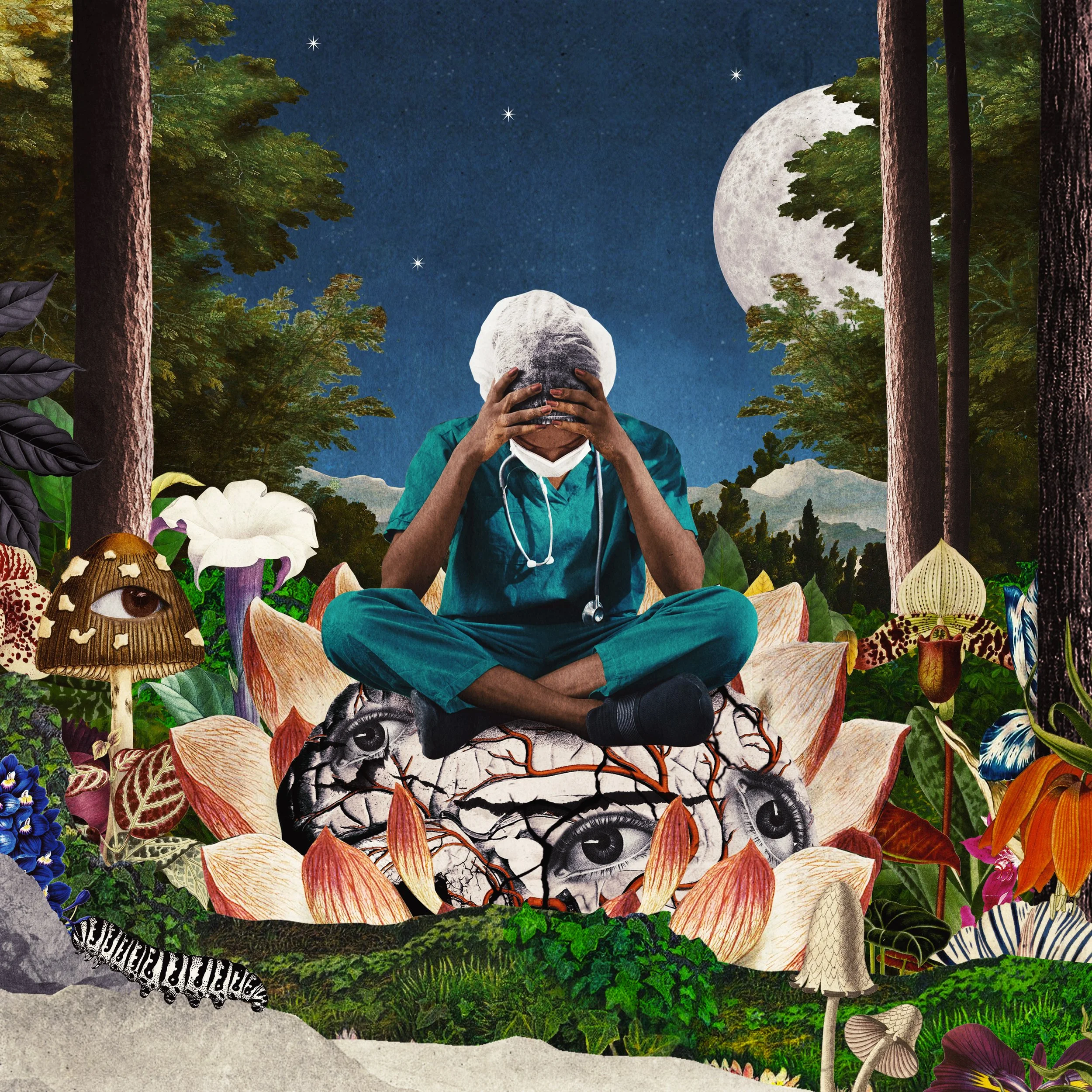
What is shame? And how does it manifest in medical culture? In this episode, The Nocturnists teams up with shame researchers Will Bynum and Luna Dolezal to investigate these questions. From a pool of over 200 stories submitted to The Nocturnists from healthcare workers across the US, the UK, and beyond, we explore the tension between who we are and what the culture expects of us.
Behind The Scenes
This episode came near the end of our creative process. We tried creating it first, but it was hard to know where to begin. How do you introduce a topic as massive as shame? We knew we wanted to lay out some basic definitions, discuss why shame was important, and introduce the team. We also knew we wanted to open with Will’s shame story. It felt important that one of our “expert voices” model the courage and openness that our storytellers demonstrate throughout the series.
CONTRIBUTORS
Adrian Anzaldua, MD
Tracy Asamoah, MD
Drea Burbank, MD
Alyssa Burgart, MD, MA
Will Bynum, MD
Jennifer Caputo-Seidler, MD
Gabriel Charbonneau, MD
Luna Dolezal, PhD
Alice Flaherty, MD, PhD
Margaret Leddy, PA-C
Erin Loeliger, MD, PhD
Alessandro Racioppi
Cynthia Shortell, MD
And other healthcare professionals who wish to remain anonymous
PRODUCTION TEAM
Host & Co-creator: Emily Silverman, MD
Co-creators & Research Leads: Luna Dolezal, PhD & Will Bynum, MD
Producer, Editor & Audio Engineer: Sam Osborn
Producer & Assistant Editor: Molly Rose-Williams
Additional Producing: Adelaide Papazoglou
Production Coordinator: Penelope Lusk
Medical Student Producers: Corinne April Iolanda Conn, MPH & Nikhil Rajapuram, MD
Impact Campaign Manager & Assistant Producer: Carly Besser
Executive Producer: Alison Block, MD
Chief Operating Officer: Rebecca Groves
Exeter Team Coordinator: Alice Waterson
Series Illustrator: Beppe Conti
Music: Blue Dot Sessions
SPONSORS
This episode of The Nocturnists is sponsored by #FirstRespondersFirst, a fund of the Entertainment Industry Foundation (EIF), a 501(c)(3) charitable organization.
Shame in Medicine: The Lost Forest is made possible in part by the Shame and Medicine project at the University of Exeter, funded by the Wellcome Trust.
The Nocturnists is supported by the California Medical Association, and people like you who have donated through our website and Patreon page.
-
Download the discussion guide for Episode 1, "Hello, Shame" here.
-
LISTEN:
The Nocturnists podcast, Conversations: Cathy O’Neil on The Shame Machine.
Thales Well podcast, On Shame with Luna Dolezal.
See Hear Feel podcast, Dr. Luna Dolezal on shame in medicine.
READ:
A Better NHS – Blog by UK National Health Service (NHS) General Practitioner Jonathan Tomlinson exploring the relationships between doctors and patients and health policy. See posts on Shame, Empathy and Shame, Shame and Redemption, and Empathy, Shame and Medical Professionals.
Shame Glossary (work in progress). Shame and Medicine project.
Aubin D. King S. The Healthcare Environment: A Perfect Ecosystem for Growing Shame. Healthc Q. 2018 Jan;20(4):31-36.
hooks b. Moving Beyond Shame. Teaching Community: A Pedagogy of Hope. 2003.
Davidoff F. Shame: the elephant in the room. Qual Saf Health Care. 2002 Mar;11(1):2-3.
Dolezal L. Gibson M. Beyond a trauma-informed approach and towards shame-sensitive practice. Humanit Soc Sci Commun 9, 214 (2022).
Gilbert P. Shame and the vulnerable self in medical contexts: the compassionate solution. Medical Humanities 2017;43:211-217.
Lazare A. Shame and humiliation in the medical encounter. Arch Intern Med. 1987 Sep;147(9):1653-8. PMID: 3632171.
Lyons B. Gibson M. Dolezal L. Stories of shame. Lancet. 2018 Apr 21;391(10130):1568-1569.
Ofri D. Chapter 5, Burning with Shame. What Doctors Feel: How Emotions Affect the Practice of Medicine. 2014.
WATCH:
The Shame Conversation, prod. Will Bynum, MD.
UCL Centre for Perioperative Medicine, Shame… An Interview with Dr Jonathan Tomlinson.
-
The Nocturnists – Shame in Medicine: The Lost Forest
Ep. 1 Hello, Shame
Episode Transcript
Note: The Nocturnists is created primarily as a listening experience. The audio contains emotion, emphasis, and soundscapes that are not easily transcribed. We encourage you to listen to the episode if at all possible. Our transcripts are produced using both speech recognition software and human copy editors, and may not be 100% accurate. Thank you for consulting the audio before quoting in print.
Will Bynum
I'm in the early part of my second year of family medicine residency training, and I'm sitting in the labor and delivery workroom watching the clock go by, to get to the end of my long 24 hour shift. It's always a little eerie, or unsettling, for it to be too quiet on a Labor and Delivery unit. Almost like you're just waiting for the other shoe to drop, and all hell to break loose. And it did.
I hear a lot of commotion on the other end of the hallway. And I stick my head out the door and see a woman, clearly in a lot of distress, being quickly shuffled into a room. And a minute later, the obstetrician sticks her head out the door, and calls for me to come to the room to get involved in her care. And I enter a room that is tense. There are multiple nurses; there's an obstetrician; there's a pediatrics team. And clearly there's something major going on. And despite the chaos, it seems like everyone knows what they're doing. Except for me. I'm feeling insecure, as I had the entire rotation, and feeling a little panicked at being involved in the situation without a lot of skills.
The obstetrician pulls me over to the patient and tells me that she's having a placental abruption, which is where the patient's blood supply to the baby has been disrupted and the baby is in distress. The urgency in the room was to deliver it as quickly as possible. And so we did that using a vacuum-assisted device, which is where you attach a small cup to the baby's head, and the person delivering her, gently but deliberately, pulls the baby out of the mother's body. Almost in a daze, as if I was watching myself from across the room, I found myself at the foot of the bed, pulling the baby out of the mom's body and praying silently that everything would go okay.
And it didn't. I deliver the baby successfully, thank God, but in the process, I cause injury to the mother. One of those events that you live in fear of – as a resident, as a physician – where you, and everyone around you (and there were a lot of people in the room), know that something has just gone terribly wrong. And it's almost like time stopped. And, I can feel my heartbeat in my ears; I can feel my guts falling on the floor; I can feel my temperature rising. I feel incredibly uncomfortable and incredibly exposed. Like I was standing under a bank of those hot, bright operating room lights, and the rest of the room around me is dark. And there I am: panicking.
And what I see are the eyes of the people standing around me, 'til I see, and I feel, the judgment. And the only thing I know to do in that moment – some sort of subconscious primitive impulse – is to leave the room. And I do that. Which is not something I would usually do, or have ever done. But I left. I handed the baby off; I handed the vacuum device off, and I literally left the room in the middle of the situation.
And when I get out in the hall, I'm disoriented, and I just start walking. And the only thing guiding where I go next is the desire to get as far away from that room, that mom, that baby, the nurses and the obstetrician, as possible. And after walking through what feels like a maze of hallways in the hospital, I find myself on the complete other end of the hospital, in (of all places) a meditation room: by myself, in the corner, back against the wall, slumped down on the floor, head in hands, behind a chair. Literally hiding. And, as bad as that emotional experience was, I was not prepared for the shame that was coming.
Emily Silverman
You're listening to Shame in Medicine: The Lost Forest. I'm Emily Silverman. In August 2020, I got an email from a philosopher in the United Kingdom. It was from Luna Dolezal: "Yeah Emily, my name is Luna Dolezal." Luna wanted to know if we could collaborate on a podcast on the theme of shame in medicine. She told me that she'd been listening to the podcast for a while, and she noticed that shame kept coming up again and again in the episodes.
Luna Dolezal
So one thing I found, listening to the other series of The Nocturnists – Stories from a Pandemic and Black Voices in Healthcare – I just heard shame coming up over and over again in these stories. There are stories about not fitting in, not feeling good enough; stories about mistakes and failure, feeling inadequate in different ways. And what was really interesting was like, shame was coming up over and over again. But also, at the same time, it was never actually spoken. So shame was like this present absence in many of the stories I heard. And it's one of the things I said to Emily is, like, people are talking about shame, but nobody's saying the word “shame”. Like, we're not naming this affective or emotional force, that is having such a profound impact on people and what they're up to in healthcare.
Emily Silverman
After talking to Luna, I started to see shame everywhere in medicine. How many times had I felt ashamed at work? Ashamed for making a mistake? For cutting corners or rushing an interaction? For not knowing enough... for knowing too much? For getting tired, for getting sick?
Luna Dolezal
And so, it was kind of, like, bringing the subterranean, or what's underground, to light; bringing it up to the surface, by actually naming the shame. And, just, let's just have the stories be about shame. And let's just get that out in the open and see what comes up.
Emily Silverman
So, after talking to Luna, I got really excited to explore this topic of shame in medicine. We announced a call for shame stories. I received almost 200 submissions from healthcare workers across the United States, United Kingdom, and beyond.
Tracy Asamoah
He presented it in a way that said, "You should have known this; you missed something big." And at that moment, I felt my stomach drop, and felt like I wanted to sink into the floor...
Josh
We decided to go on a walk. And I remember, as I was walking with my family, that I kept looking over my shoulder, thinking that someone was coming after me...
Drea Burbank
Like I said, I felt like I got a golden ticket: Charlie in the Chocolate Factory ticket, and to show up at the chocolate factory and be told that everything about you is wrong.
It felt like I had slammed into a brick wall, going 60 miles an hour...
Jennifer Caputo-Seidler
Underneath my gown and my mask, I'm starting to sweat. I feel my face flushed. And I'm very grateful to be wearing that mask, so that he can't see how humiliated I am. And in that moment, I feel so powerless.
Anonymous
Now, I'm not this person. I've never been this person. And I think, in this moment, I am going to have to hide myself. I am going to have to become someone that I am not, if this is what the standard is.
Anonymous
It was palpable in the air. I felt my cheeks turning red; felt my legs about to give way beneath me. I had no response. I've replayed that moment over and over and over again in my mind.
Gabriel Charbonneau
When I think about this, the words just sort of go away. It's almost like there's a protective mechanism that's tripped off that says, "Hey, that's not something that you should be talking about."
Gayle
I remember seeing the people walking by me, like just hundreds of people you walk by in the hospital, and I wondered how many of them knew that I had done this terrible thing.
Erin Loeliger
Shame casually falls onto my shoulders, least expected – wrapping tighter and tighter. Feeding on my confidence sucking away my breath, paralyzing me to the spot. Others ask: "What's wrong?" How can I answer them? I smile and say, "I'm fine."
Emily Silverman
Over the course of this 10-episode season, you'll hear many of these shame stories and also from Will and Luna, our shame experts, who have devoted their careers to studying this phenomenon. Back to Will.
Will Bynum
So when I left the patient's room and found my way into this meditation room, I was having a lot of just acute emotion. And as that died down, these different feelings started to creep in, and they were driven by, really what was a voice in my head, that prior to that point, and prior to this error, had been whispering, "Are you really good enough to be here?" "Are you the strong resident that you're seen to be?" It was a quiet questioning, that was coming from the voice in my head, that I could usually drown out. But now that voice was screaming at me. I mean, it was, it was yelling.
And they were beliefs that I had about myself: you are not competent enough; you are unworthy; you are a bad doctor; you're a bad person. You know, I'd come to know myself as, at least, a resident who is willing to work hard and, increasingly, who is worthy of being trusted. In a moment that was just gone, evaporated. For a while, I mean days, it was an unimpeded voice. There was no counter-voice. There was no logic or rational thinking or perspective that I could come up with, that would tell that voice it was wrong, or overly harsh, or inappropriate. So, for a while, I just believed it. And that was the sort of the depth of the shame.
The recovery was not quick, and it was not easy, partly because I didn't know what I was experiencing. I didn't know what I was feeling. Part of the acceleration of that sort of decay, if you will, the shame, I achieved through reaching out to other people. I mean, I met one of my best friends, who was in my residency class, for breakfast a few days later, and he was the first person I told about it. That was very helpful. I mean, it was helpful just to bring some sort of release into that situation. But the most important thing that did, was it allowed him to say, "I think this was just an unfortunate outcome that could have happened to anybody." That was huge for me, because up to that point, all I was seeing was my own inadequacy, my own failure, my own transgression.
And what he helped me see was that it wasn't just me. That there was a circumstance and a situation, and something that may have been somewhat out of my control. And, so it actually took me out of a very self-centered place, centered on my own distress, and into a place where I could see myself more objectively. And then for the first time, I was able to think, "Oh God, I mean, what about the patient?" I never went and showed my face to the patient, which was so far outside of my values. And as it turns out, I later found out through a colleague, she was... she wanted me to come by. She was looking for me because she wanted to thank me, you know, for helping to save her baby in an emergency situation. So that experience of sitting down and talking to someone about this, and having that perspective, was huge. And then over time, I just had to come to see myself as, you know, imperfect person who makes mistakes, but is willing and able to learn from them.
Emily Silverman
Will is a Family Medicine doctor, residency program director, and associate professor of Family Medicine at Duke. And the shame experience he just described was so potent for him that it inspired him to dedicate a large portion of his academic research to studying shame in medical learners. Luna Dolezal, the philosopher whose voice you heard earlier in this episode, got interested in shame a different way.
Luna Dolezal
I became interested in shame in medicine through thinking about athletic surgery or cosmetic surgery.
Emily Silverman
Initially, she was studying shame and the body, specifically the shame that leads women toward plastic surgery, and the way physicians might kindle or reinforce that feeling of shame. But then, she met a physician from Dublin named Barry Lyons.
Luna Dolezal
He was, like, you know, shame is everywhere in medicine; we need to do a project about this.
Emily Silverman
Luna and Barry started talking about how shame circulates: not just between doctor and patient, but in the medical culture at large. And so they, and some of their colleagues, launched a project to explore these deeper, more fundamental forces, called the Shame and Medicine project. Before we dive into the stories, I wanted to share some insights about shame that I got from my conversations with Will and Luna. Because as healthcare workers, who doesn't love a little bit of learning?
First, shame is an emotional experience that we have when we feel like our social bonds are threatened. Maybe we've made a mistake or transgressed in some way, and shame serves as a warning signal, almost like a pain response, that alerts us that we've compromised our relationship to others. It's a super primal emotion, that probably evolved to keep us in the herd, which means that it's not logical. It's about survival.
Second, there's a family of emotions called self-conscious emotions. And shame is one of them, along with guilt and pride. Built into these emotions is someone else's point of view. In other words, to experience shame, we have to see ourselves through someone else's eyes, which isn't necessarily true with other emotions like happiness or sadness or anger. Interestingly, this external observer doesn't even have to be real. It can be abstract or imagined or even internalized. You don't even have to agree with this other point of view, in order to feel shame about it. What makes shame interesting is that social norms and expectations are rolled into the emotion. It serves as a bridge between the personal and the collective.
Third, there's a very specific phenomenology to the acute shame experience. Usually, the way it works is: You do or say something shameful, that's witnessed by others. And there's this response that happens at the level of the body. There's a feeling of everyone looking at you, a feeling of being super visible. And actually, the body agrees: blood rushes to the face. Often there's a sense of time stopping or desire to be swallowed by the ground. The body folds in on itself: the shoulders slump; the head hangs. And all of this is associated with intense feelings of self-disgust, unworthiness, and unattractiveness, in the eyes of others. These experiences are so powerful that we can vividly relive them days, or even years, later. People actually call shame the emotion of social control, because people will bend over backward to avoid shame. Therefore, the emotion drives behavior in a way that other emotions don't.
Lastly, shame is a shape-shifting emotion. What's shameful for you might not even register for me, and vice versa. It all depends on the person's history, and the culture that surrounds them.
And that brings us to the idea of chronic shame, or shame-proneness. This is where you've felt shame so many times over the course of your life, that you actually just come to expect it. And you might even feel it come up in response to a scenario that others consider normal. In other cases, we might have become so good at avoiding shame, that we don't even feel the shame anymore. But rather the consequences of the habits or behaviors we've developed to avoid it, like self-attack, or rage, aggression, violence, avoidance/withdrawal.
Now, there's a lot of literature out there about the emotion of shame in general, but other than Will and Luna's research, there's almost nothing about shame in medicine, even though healthcare might be one of the most shame-prone fields out there. After all, a big part of our job in health care is discerning between what is normal and abnormal, what is healthy or pathological. In this series, we focus primarily on how clinicians shame themselves and each other. Though we don't focus explicitly on the patient experience, these stories have direct implications for patient safety and well-being.
Luna and Will, what are the goals of this project?
Luna Dolezal
So first, we wanted to create a forum where people could share their shame experiences. So shame really thrives on secrecy. And, one of the things about shame is, if you bring it out into the open, it can really defuse shame. It can be really cathartic and connecting to share your story.
Anonymous
I've wanted to be a doctor for as long as I can remember.
Margaret Leddy
The story begins when I was a PA student.
Anonymous
This is a story about a complication, anatomy, shame, and interventional radiology.
Umme F.
My story dates back to last year when I was in the hospital for 27 to 30 hours straight, on a really hectic shift...
Will Bynum
We also wanted to create a shared vocabulary around shame experiences, so that when those of us in the healthcare profession experience shame, we have a label for what it is that we're going through. Shame can be a very disorienting emotional experience, and being able to identify it, and name it in a moment, can be a really helpful and powerful thing.
Alice Flaherty
I didn’t bother to label it as shame because it was just so immediate… I was in the thrall of these emotions and it was almost a physical sensation… it was just like being ripped by my own actions, or rotted… it was that kind of decay.
Luna Dolezal
Third, we wanted to use shame as a lens through which we could examine medical culture. So, when you focus on shame experiences, what it shows you is the kind of contours of that culture. So shame tells us when something is acceptable or unacceptable; when something is proper or improper; when something is valued or it's not valued at all. So, using a shame lens can really tell you lot about a culture – kind of reveal its boundaries and its contours.
Anonymous
It’s always something that I walk into the room knowing that people are going to see and make assumptions about, and does not feel like something that I have the current capacity to have a conversation with them about, to say that the fact that I’m fat and a doctor is actually a pretty remarkable thing.
Will Bynum
Last, and maybe most important, we want to use this series as a platform for inviting discussion, sharing, and ideas about how we can transform that medical culture. But being able to identify, and discuss, and manage our shame, proactively, as individuals, and as a community of people, is going to be vital if we want to create a healthy and sustainable culture, both for us as healthcare professionals, as well as the patients we serve.
Emily Silverman
Now, we received way more shame stories than we had time to include in the series. We did our best to cluster the stories by theme. The front half of the series focuses on shame experiences that come up as we're breaking into the profession. What are our backgrounds? What about testing and applications and training and learning everything we need to learn to become who we are in the medical profession? The back half of this series is about shame experiences that come up once we're already practicing. How do we deal with mistakes? How do we handle difficult situations like getting sued? Toward the end, we'll be exploring how these stories might help us imagine a new medical culture, one that's grounded in belonging.
Thanks for listening to Shame in Medicine: The Lost Forest. In addition to just listening to the series, there are so many other ways to engage. If you visit our website at thenocturnists-shame.org, you can submit a reaction or reflection to the series, check out the discussion guides we've made, or even find information about how to organize a gathering, whether it's formal or informal, to start a conversation about shame in your community. We're really excited about these free resources, which we've never developed before, to accompany our projects, and hope that you find them useful.
Next week, we'll be exploring the theme of the "ideal doctor". What is the ideal doctor? Where did those ideals come from? And how do those ideals serve us, or harm us? Tune in to The Nocturnists next week for more of Shame in Medicine: The Lost Forest.
Shame in Medicine: The Lost Forest was co-created by me, Emily Silverman, as well as Will Bynum and Luna Dolezal. Our producers are Sam Osborn and Molly Rose-Williams, with additional producing by Adelaide Papazoglou. Sam also edited and mixed the series. Thanks to Medical student producers: Corinne April Iolanda Conn and Nikhil Rajapuram. Production Coordinator: Penelope Lusk. Impact campaign manager and Assistant Producer: Carly Besser, and Exeter team coordinator Alice Waterson. The Nocturnists Executive Producer is Ali Block, and our Chief Operating Officer is Rebecca Groves.
The series illustrations are by Beppe Conti, and the music comes from Blue Dot sessions.
Shame in Medicine: The Lost Forest was made possible in part by the Wellcome Trust and the Shame in Medicine project at the University of Exeter.
The Nocturnists is supported by the California Medical Association, a physician-led organization that works tirelessly to make sure that the doctor-patient relationship remains at the center of medicine. To learn more about the CMA, visit cmadocs.org.
Our show is also made possible with donations from listeners like you. Thank you so much for supporting our work in storytelling. If you enjoy the show, please follow us on your favorite podcast app so you don't miss an episode. While you're in there, you can help others find us, by leaving us a rating and review. To contribute your voice to an upcoming project or to support our work with a donation, visit our website at thenocturnists.com.
I'm your host, Emily Silverman. See you next week.